A thin fibre-optic telescope (arthroscope) is passed into the knee joint to be able to visualise the inside of the knee on a television monitor.
Intra articular damage can be diagnosed, assessed and treated. Many knee conditions including meniscus surgery and repair , treatment of cartilage damage , removal of loose fragments, treatment of the patella with /without lateral release and also removal of inflamed joint membranes can be treated arthroscopically . ACL-reconstructions and other knee ligament repairs or reconstructions are also done with the help of an arthroscope.
The Procedure
Knee arthoscopy is usually performed under general anaesthetic as a day procedure.
Two or more very small incisions on the outside of the knee are used to allow the insertion of the arthroscope and instruments into the joint. For safety, I usually use a small suture to close the portals after surgery. These very small puncture holes (portals) which usually heal within 1 week .
Meniscus Tears
There are many possible injury mechanisms , however most tears are caused by either twisting or squatting.
Pain is felt on the inside, outside or back of the knee.
The torn fragment can cause pain, locking or clicking and also damage to the overlying cartilage in the knee joint.
In most situations the torn piece of meniscus is removed.
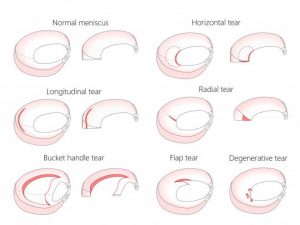
Above: Different types of meniscus tears
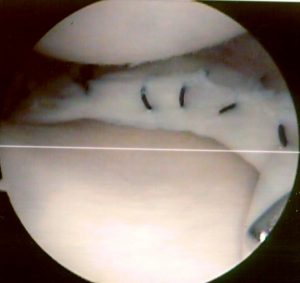
If there is good potential for healing, the meniscus is repaired with sutures as seen below.
Degenerative Meniscal Tears
Click here to read The Australian Knee Society guide
Cartilage Damage
Loose floating cartilage fragments can cause sharp pain and locking of the knee.
Damage to the surface of the knee can cause increased friction, swelling and pain. Generalised cartilage wear can lead to painful arthritis.
In some instances, larger full thickness cartilage defects can be successfully grafted (autologous chondrocyte grafting). For small defects the ‘Nano (Micro) Fracture technique’ has been shown to result in fibro-cartilage healing.
Most commonly the aim of surgery is to remove loose fragments and to smoothen rough edges of de-laminating cartilage.
Patella Treatment
In many cases “anterior knee pain” can be treated successfully without an operative intervention. For Patella Maltracking a combination of strengthening of the medial Quadriceps Muscle (VMO=Vastus Medialis Oblique) , patella taping and patella brace can be helpful. Jens is happy to direct you to the most suitable Physiotherapist to work with you and achieve the best possible results.
If all non-operative measures fail to relieve symptoms, patella re-alignment surgery with/without arthroscopic ‘Lateral Release’, with/without reconstruction of the MPFL (Medial Patello Femoral Ligament) and with/without tibial tuberosity transfer may be indicated. Damage to the patella cartilage can be treated by smoothing , cartilage grafts are usually not successful in this location.
Risks
Knee Arthroscopy is safe and effective , but has as with all surgery there are risks.
- Infection : Rare < 0,3%, can be a serious complication requiring antibiotic treatment and further surgery with wash out of the knee.
- Bleeding and bruising into the knee or leg.
- Blood Clots in a deep leg vein (DVT) – life threatening clots have been reported in the literature, but are rare.
- Numbness near the incisions is common, but usually disappears over time.
- Injury to blood vessels and nerves are extremely uncommon.
- Synovial fistulas are usually avoided by using a suture for the small skin incisions.
- In general the risk of any major problems is less than 1%
General Protocol for Rehabilitation and Physiotherapy
In Hospital:
- You will be given instructions with exercises to speed up your recovery and strengthen your leg muscles, a physiotherapist will guide you through the exercises.
- Usually Full Weight Bearing, for comfort, crutches or other walking aides may be used
- Waterproof dressings are usually applied
At Home:
- Keep the wounds dry
- The outer bandage may be removed after 24 hours
- The waterproof dressing should remain intact unless you notice ooze or if water leaks under it, in which case you should replace e dressing with clean dry ones.
- You may have some swelling and bruising which is normal.
- Apply principles of RICE – Resting your leg as often as needed
- Ice packs 3-4 times a day
- Compression- wear tubigrip during the day only, remove at night.
- Elevate your leg when sitting /lying down
- You will be given pain medication to take as directed and if needed.
- Do gentle leg exercises (straight leg raises and knee bending) as per instruction sheet and as tolerated
- Weight bear as tolerated
Follow-up review :
- Usually 5-10 days post op to monitor progress
Stitches will be removed at follow-up visit
Return to activities:
Let pain be your guide, if you experience increased pain, you are doing too much.
Sport
- Light training, Cycling and Swimming usually 2-3 weeks post surgery
- Return to running and ball sports should be discussed with Jens, as this will depend on details of your surgery
Driving
- You will be able to drive when comfortable
Work
- You may return to work after 2-3 days if you work in an Office
- For return to more physical work, 3-6 weeks